Cornea Surgeons In Tallahassee, FL
The cornea is the outermost part of your eye and extremely important for clear vision and overall eye health. Your cornea is a transparent covering over the front part of the eye, much like the watch crystal on your watch. It covers your iris, pupil and anterior chamber. The cornea serves multiple purposes, forming a protective barrier against germs and dirt, filtering out ultraviolet rays and helping to refract light, an important component of vision.
There are three main components of the cornea:
- Endothelium
- Stroma
- Epithelium
The epithelium provides an important protective barrier to infection. Anything that compromises the epithelium can increase the risk of corneal ulceration, such as abrasion of the cornea, or hypoxia resulting from overwear or sleeping in contact lenses. The endothelium is the innermost layer of the cornea and consists of a single layer of cells between your stroma and a clear fluid located in the front and rear chambers of your eye called the aqueous humor. Your endothelium acts as a pump, helping to remove water that is absorbed into your stroma. If the endothelium doesn’t work properly, your stroma can become hazy, causing your vision to become fuzzy.
What Is A Corneal Transplant?
A cornea transplant, also known as a corneal graft, or as penetrating keratoplasty, involves the removal of the central portion (called a button) of the diseased cornea and replacing it with a donor button of the cornea. Corneal grafts are performed on patients with damaged or scarred corneas that prevent acceptable vision. This may be due to corneal scarring from disease or trauma.
When Should I Have A Corneal Transplant?
A common indication for keratoplasty is keratoconus. The eye-care practitioner must decide when to recommend keratoplasty for the keratoconic patient. This is often not a simple, straight-forward decision.
Keratoplasty for keratoconus is highly successful; however, there is a long recovery period and a risk of severe ocular complications. A number of factors must be considered in deciding when to do a keratoplasty. One of the most important is the patient’s functional vision. If the best acuity with their contact lenses prevents them from doing their job or carrying out their normal activities, a transplant must be considered. The actual measured visual acuity may be quite different for different patients. One patient may find that he/she can not do their job with 20/30 acuity while another patient may be very satisfied with 20/60 acuity. Very careful and specialized contact lens fittings are necessary before recommending a corneal transplant.
One study found that 69% of keratoconus, most referred for transplant, could be successfully fit with contact lenses if special lens designs were used. Thus, prior to transplant, every effort should be made to optimally fit the patient with contact lenses, especially if there is not significant corneal scarring affecting vision. However, a few patients become intolerant to contact lenses and require a transplant earlier than otherwise would be necessary. If the patient has a large area of thinning, a very decentered cone or significant blood vessel growth into the usually clear cornea, called neovascularization, a transplant may be performed earlier than otherwise indicated by the visual performance, as these factors may require a larger than normal transplant button size and/or increase the chance of rejection if allowed to advance too far. It is important to realize that a transplant does not necessarily guarantee freedom from contact lenses, as they are often required for resulting refractive errors and astigmatism.

Healing After Corneal Transplant
The healing process following transplant is long, often taking a year or longer. The time from surgery to the removal of the stitches is commonly 6 to 17 months. The patient may be on steroids for months. Initially following surgery the donor button is swollen and even following healing the button is usually thicker than the corneal bed in which it rests. The photo on the left shows a thick white ring of scarring between the donated button and the patient’s outer cornea. The white radial marks are where stitches were placed to hold the transplant in position. Graft rejection reactions occur in 11% to 18% of the patients. Signs of graft rejection include ciliary flush, anterior chamber flare, keratic precipitates, Khodadoust line, and Krachmer’s spots. Signs of graft rejection are reported to occur from 1 month to 5 years following surgery. Symptoms of rejection noticeable to the patient include redness, light sensitivity, pain or blurry vision. The rejection rate for bilateral grafts is higher than if only one eye is grafted. In the bilateral cases, when a rejection reaction occurs it is common in both eyes. If the second eye is to be grafted, there is usually a period of at least a year between grafts. If signs of rejection occur, aggressive treatment with steroids is begun. Usually, the reaction is overcome and the graft remains clear. Over 90% of the corneal grafts are successful with some studies reporting 97% to 99% success rates at 5 and 10 years. Large amounts of astigmatism are common following keratoplasty.
Keratoconus
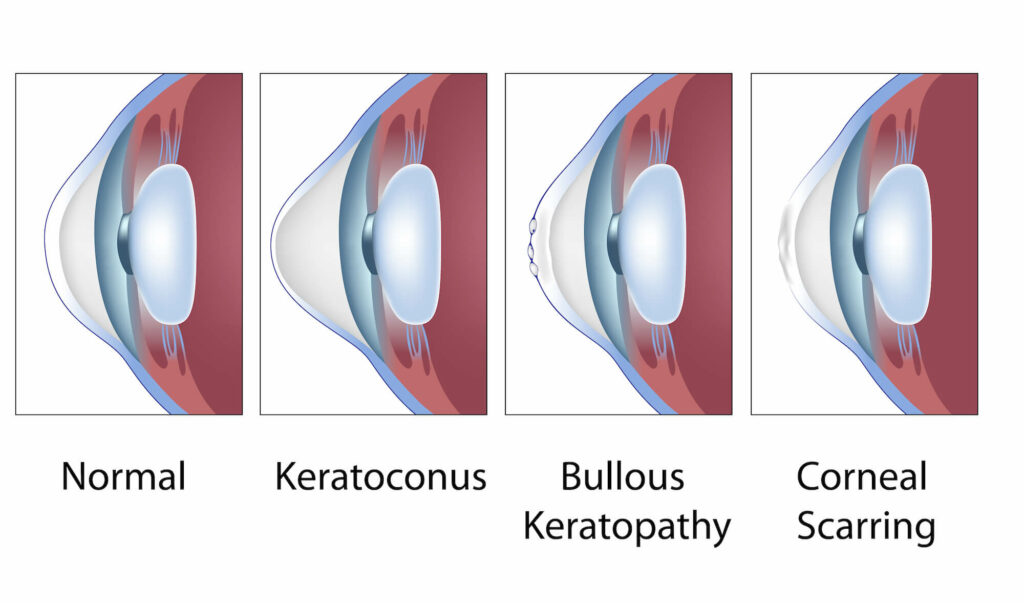
Keratoconus Definition – An eye disorder characterized by an irregular corneal surface (cone-shaped) resulting in blurred and distorted images.
The cornea is the window and outer surface of the eye. When you are visualizing an image, light travels through the cornea, then through the lens to the retina and then on to the brain to form a visual image. The normal corneal surface is smooth and dome-shaped and aspheric (flattens towards the edges). Light rays passing through it move in an undistorted manner to the retina to project a clear image to the brain. This is the typical normal working cornea.
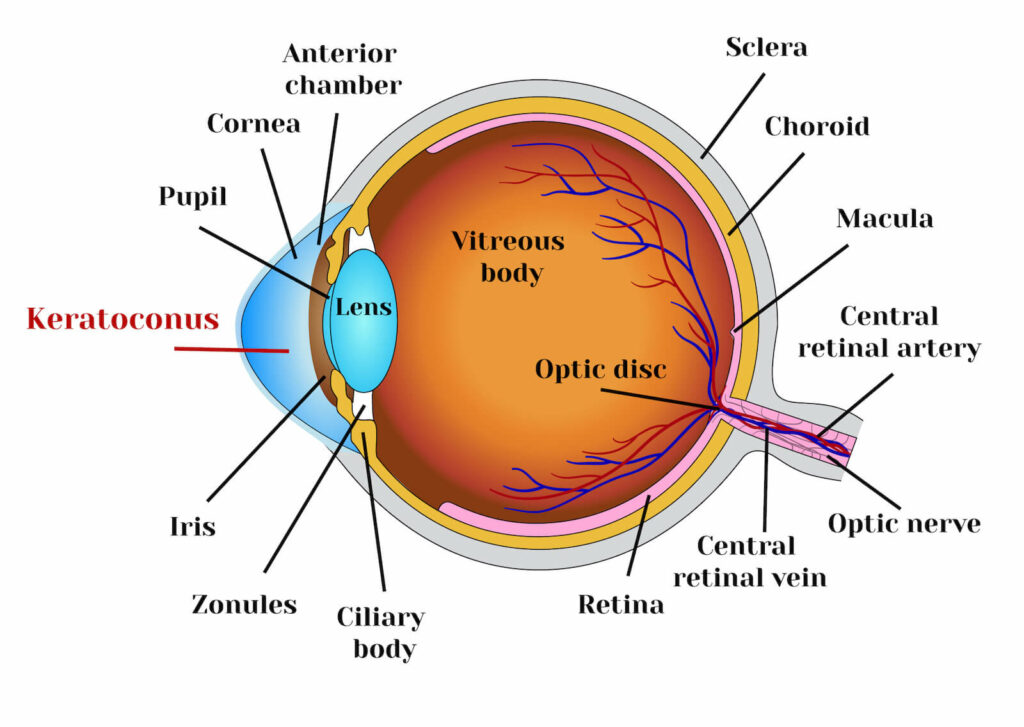
Keratoconus is a progressive eye condition that affects the cornea. The normally round, dome-shaped cornea weakens and thins, causing a cone-like bulge to develop. The regular curvature of the cornea becomes irregular, resulting in increasing nearsightedness (myopia) and astigmatism that have to be corrected with special glasses or contact lenses. Since the cornea is responsible for refracting most of the light coming into the eye, corneal abnormalities can result in significant visual impairment, making simple tasks difficult like driving or reading.
Symptoms of Keratoconus
- mild burning
- glare at night
- irritable eye
- sensitivity to light
- some distortion of vision
According to the American Academy of Ophthalmology, about 1/2000 people will develop keratoconus. Most people will have a mild or moderate form of the disease. Less than 10% of people with keratoconus will develop the most severe form. It typically is diagnosed in the late teens or twenties, however, many people have been diagnosed in their mid to late thirties. It is common for one eye to progress faster than the other and the eyes may go for long periods of time without any change and then change dramatically over a period of months. Rubbing the eyes is known to hasten progression, and modern treatments such as Intacs and collagen cross-linking may delay progression.
Fuchs’ Dystrophy
Fuchs’ dystrophy is an inherited disease of the cornea in which the innermost layer of the cornea, called the endothelium, becomes dysfunctional and may result in decreased vision. The front part of a normal eye is filled with a fluid called the aqueous. However, the cornea, which separates the outside air from the aqueous fluid inside the eye, must maintain a proper balance of moisture in order to maintain its clarity. To accomplish this task, the inside of the cornea is lined with a specialized layer of cells called the endothelium. The endothelial cells function as one-way pumps, drawing fluid out of the cornea and pumping it back into the eye. By so doing, the cornea, despite being in direct contact with the aqueous eye fluid, doesn’t become overly hydrated and maintains clarity.
In Fuchs’ dystrophy, the endothelial cells are slowly replaced with small collagen bumps called guttata. Guttata may first appear in the cornea in the 20s and 30s, though rarely cause any symptoms until later in life. As a person ages, the guttata may slowly increase in number and size. In the process, the endothelial cells surrounding them may slowly die. When a critical number of endothelial cells are lost, usually by the age of 50 to 60 years, the pump function of the endothelium may be overwhelmed and the cornea starts to swell with eye fluid. As the swelling worsens, the vision may start to decrease. In cases where large amounts of guttata exist on the cornea, the vision may also become compromised even without corneal swelling from an irregular scattering of light passing through the dense guttata layer.

Cause Of Fuchs’ Dystrophy
Fuchs’ dystrophy is caused by an inherited malfunction in the way the inner lining cells of the cornea behave. The gene is transferred from parent to child in an autosomal dominant fashion, which means that each child of an affected parent has a 50% chance of developing the disease. Though many family members may have Fuchs’ dystrophy, its effects may vary greatly from one family member to the next. As such, some individuals with Fuchs’ dystrophy will have signs of the disease visible only to a doctor examining their corneas with a slit lamp, and will never suffer any visual loss from the disorder. Other individuals who have worse forms of the disease may suffer slowly progressive visual loss.
Symptoms Of Fuchs’ Dystrophy
Fuchs’ dystrophy is usually asymptomatic until a person reaches 50 to 60 years of age. For individuals with worse forms of the disease, the endothelial cells of the cornea may become so compromised enough that the cornea begins to swell with eye fluid. This swelling is usually gradual over many weeks or months and maybe so slow that it is not immediately noticeable. When the swelling becomes advanced enough, a person may notice that the vision seems not as sharp as it used to be. The vision may often be worse in the morning, due to swelling of the cornea overnight, and improve as the day goes on while the eyes are open and exposed to the drying effect of the air. Fuchs’ dystrophy patients may also complain of more glare in sunlight conditions and more difficulty seeing in low light conditions. As the swelling becomes severe, the vision may decline greatly, causing true impairment of a person’s daily living activities.